Arthritis and arthritis are diseases characterized by pathological changes in the joints, but the difference between arthritis and arthrosis is important. To understand the difference between arthritis and arthrosis, it is necessary to consider the etiological factors, pathogenesis, and symptoms of arthritis and arthrosis. The treatment of arthrosis and arthritis also has different approaches.
What is arthritis, arthrosis? How do joint injuries manifest themselves in arthritis and arthrosis, what is the difference? Differences in arthrosis and arthritis are related to the mechanism of pathological changes.
Treatment of arthrosis and arthritis is long-term, multicomponent. Arthritis and arthrosis can be considered consecutive stages of the pathological process as a result of not being treated in time. After understanding what arthritis and arthrosis are, we will determine the differences between arthrosis and arthritis.
Arthritis, classification
Arthritis - due to inflammatory changes, includes the pathology of the joints, and is a symptom of other diseases that occur with their defeat. How to treat arthritis depends on determining the cause of the inflammatory process.
According to the etiological factor, there are the following:
- Primary - rheumatoid, rheumatoid arthritis, ankylosing spondylitis, Still's disease and others.
- Secondary - complications of an infectious, non-infectious process (chlamydial infection, hepatitis, diseases of the gastrointestinal tract, reactive with septic lesions).
According to the number of joints affected:
- Monoarthritis - with the defeat of a single joint.
- Polyarthritis - when a group of joints is affected.
According to the nature of the course of the disease:
- Acute arthritis - with a bright clinical picture of inflammatory changes in the connective tissue of the joint.
- Subacute - an intermediate option, the stage of resolution of the acute situation.
- Chronic arthritis - an erased clinical picture, a slow course, with periods of weakening and exacerbation.
Osteoarthritis, classification
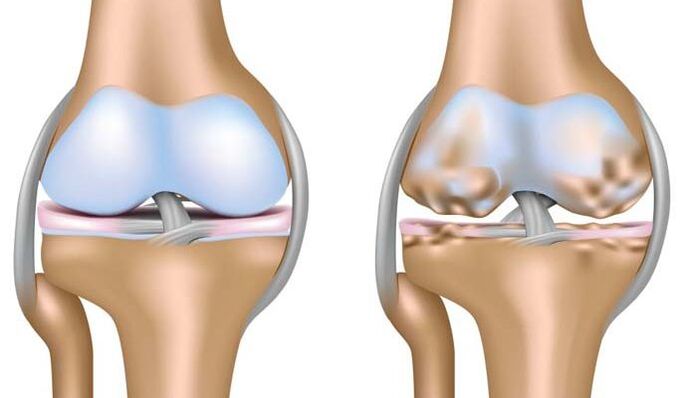
Deforming osteoarthritis, rheumatoid arthrosis or arthrosis is a disease based on degenerative changes associated with the destruction of all joint structures, cartilage, ligaments, muscles, tendons and bones. This is the main difference between arthrosis of the joints and arthritis, which causes irreversible deformations of the affected articular surfaces, dysfunction and disability of the patient.
- Idiopathic - no known cause. The pathological process is based on the mechanism of autoimmune damage (primary rheumatoid arthrosis in young patients).
- Secondary osteoarthritis is the result of metabolic disorders, trauma and inflammation. For example, rheumatoid arthritis after suffering from rheumatoid arthritis.
Arthritis, causes
Risk factors include:
- Disruption of metabolic processes in the body.
- Hereditary predisposition factor.
- Infectious diseases.
- Immune deficiency states, the presence of autoimmune diseases, allergic manifestations.
- Professional activity, increased load on the musculoskeletal system due to the traumatic component.
Arthrosis, causes
Risk factors for developing osteoarthritis include:
- Age. Osteoarthritis is a disease of the elderly, except for rheumatoid arthritis, which occurs in adolescence. According to WHO statistics, about 10% of the world's population suffers from arthropathy.
- Physical load, injury, excess weight that increases the joint load. Large joints suffer more than others: hip - coxarthrosis, knee - gonarthrosis.
- Hereditary factor: characteristics of metabolic processes, structure of cartilage tissue.
- Previous inflammatory processes without proper therapy.
Arthritis symptoms

Regardless of the causes of the disease, the symptoms of the disease have a similar clinical picture in the acute stage of the process and during the exacerbation of the chronic course of the disease.
- Pain is the first symptom. It has a different intensity, is more often constant, does not depend on physical activity.
- Hyperemia of the skin of the joint area, increased local temperature (the joint area is hot to the touch), open edema.
- The presence of effusion (fluid) in the cavity of the articular bag. Microbiological and cytological examination of fluid from the inflamed cavity is important for diagnosis and determines the causative factor. Knee joints are more affected. The presence of an inflammatory nature of the fluid inside the joint capsule is the difference between arthritis and arthrosis of the knee joint.
- Extra-articular manifestations of the main disease: fever, vascular damage - vasculitis, heart valves, lung diseases - alveolitis, pneumonia, kidney damage - nephritis, skin manifestations, hematological changes - anemia, increase in the number of peripheral blood platelets.
- Limitation of range of motion in the joint, dysfunction.
Osteoarthritis, symptoms

The symptoms of arthrosis are caused by a long-term lack of nutrition and blood supply to the cartilaginous plates. Cartilage loses elasticity, becomes thinner, growths from bone tissue - osteophytes form inside the joint cavity, irreversibly deform the joint surface, disrupt functionality, cause pain and significantly limit mobility.
- Pain. The onset of the disease is characterized by moderate intensity, pain, constant pain. Intensification of pain syndrome is associated with increased dystrophic changes in cartilage and deformations. The pain can change, it can be temporary: from stiffness in the morning, it becomes constant and calm during the day. A rapid, intense increase in pain is a sign of a poor prognosis.
- visible deformation.
- Functional disorders: bending, stretching.
- Characteristic creaking when moving.
- The development of joint immobility causes disability of patients.
Osteochondrosis is a common pathological condition of the spine based on the same changes in cartilage as in arthrosis.
Diagnostics

The diagnosis of arthritis and arthrosis is aimed at determining the main cause of the disease, determining the degree of activity of the process, evaluating the prognosis and effectiveness of treatment, and timely detecting complications of the disease.
The complex of diagnostic tests includes general clinical laboratory tests, instrumental studies of the liver, kidneys, X-ray diagnostic measures, microscopic, bacteriological studies.
- Distinctive features of arthritis of various etiologies are: increased erythrocyte sedimentation rate, increased level of leukocytes in peripheral blood, which allows determining the severity of inflammatory changes, increased C-reactive protein in blood plasma. - an important laboratory diagnostic test.
- X-ray examination allows you to see a characteristic picture of inflamed articular surfaces.
- MRI is the most informative method for detecting inflammatory changes within the joint capsule.
- Doppler ultrasound is used.
- In difficult cases, it is possible to perform arthroscopy for the purpose of differential diagnosis and treatment.
X-ray examination is a fairly informative method that allows you to make a diagnosis and distinguish between arthrosis and arthritis. Depending on the determined changes, the degree of deformation of the intra-articular cartilage and the width of the joint cavity, four degrees of pathological changes in arthrosis are distinguished.
Arthritis, treatment principles

The treatment of arthritis is long-term, the main goal is to treat the disease that causes inflammatory changes in the joint capsule or to achieve a long-term relapse-free course of the disease, to prevent the development of irreversible changes and deformations, and to improve the quality. and life expectancy of patients.
It is widely used to treat:
- Methods of medical action. Depending on the etiological factor, the following are used: antibacterial, non-steroidal anti-inflammatory drugs, hormones, injection of anti-inflammatory drugs directly into the joint cavity, in severe forms of rheumatic disease, chemotherapeutic drugs are prescribed.
- Non-drug treatment. Physiotherapy exercises, adherence to diet, healthy lifestyle - from smoking, alcohol, physiotherapy, timely orthopedic care and correction of existing disorders play an important role in preventing exacerbation of accompanying diseases.
- Surgical treatment is not the method of choice. This is a tool to help patients in especially difficult cases - the development of severe complications, severe pain syndrome, with the ineffectiveness of the first two methods of treatment. It has limitations and certain guidelines for appointment.
Osteoarthritis, treatment

Rheumatoid arthrosis is treated complexly, which includes:
- Non-drug treatment. Rheumatoid arthrosis treatment includes physiotherapy exercises, physiotherapy, protective regime, load reduction, diet, weight loss.
- Medical treatment is associated with pain relief. Non-steroidal anti-inflammatory drugs, hormonal drugs are prescribed more often.
- Surgical methods of treatment: plastic, arthrodesis, prostheses of large joints (knee, thigh).
Prevention of exacerbations
Due to the long, chronic course of the disease, the possibility of developing complications, regardless of the reason for their occurrence, patients are subject to constant or long-term observation, rehabilitation measures designed taking into account their individual characteristics and nature. disease.
Important preventive value are:
- Treatment of inflammatory diseases of the musculoskeletal system, a complex of rehabilitation measures after injuries.
- Limitation of loads, healthy lifestyle, proper rational nutrition as a factor in the fight against excess weight.
- Timely orthopedic correction of bone deformities acquired during life.
Remember that it is important to contact a specialist in time at the first sign of a problem. Late initiation of treatment increases the risk of possible negative consequences of the disease.



















